INTRODUCTION
Breast cancer is the most frequent cancer that occurs among women worldwide, and the second leading cause of death, claiming the lives of thousands of women each year and affecting countries at all levels of development1. About 1.67 million new cases were diagnosed and 0.522 million deaths from breast cancer occurred in 20121. Although breast cancer is rare in men, it has been estimated that 2470 men were diagnosed with breast cancer worldwide and approximately 460 die each year2. The prevalence is rising in most countries and is estimated to rise further over the next 20 years despite current efforts to prevent the disease3.The increased incidence is not surprising since there has been, in most countries, an increase in the number of women with major breast cancer risk factors. The risk factors for breast cancer include advancing age4, family history of breast cancer, early menarche, late menopause and the use of hormonal replacement therapy (HRT) with combined estrogen and progesterone5, late age of first pregnancy, few pregnancies, and short or no periods of breastfeeding. Other risk factors that could be implicated in the burden of breast cancer are obesity, alcohol consumption, and inactivity6.
The control of breast cancer in most developing countries including Nigeria and Cameroon is under the auspices of national control programs promoted by the World Health Organization and this involves educating and screening young women for clinical manifestations of breast cancer6. The earlier breast cancer is detected, the better the effectiveness of the treatment and the likelihood of survival. Breast cancer screening methods include BSE, Clinical Breast examination (CBE) and mammography, and these are usually done in combination7. Among these methods, mammography is the only one that has been proven to be effective, but the method is only cost-effective and feasible in countries with good health infrastructure4,8. BSE is the recommended method in developing countries because it is easy, convenient, private, safe and requires no specific equipment9. Its purpose is to make women familiar with both the appearance and feel of their breasts as early as possible, so that they will be able to easily detect changes in their breast. Several studies have revealed that a positive association exists between the performance of BSE and detection of breast cancer, as most of the early breast tumor detections have been self-discovered10,11.
BSE for the early detection of breast cancer is not often done by many women. Studies12,13 affirm only 17% and 12% of women, respectively, were observed to perform BSE monthly. Such an observation has equally been noted among health personnel. For instance, a study conducted among nurses and midwives reported only 14% compliance14. As a result, most cases of breast cancer in women are diagnosed at an advanced stage due to late presentation. Although BSE is a simple, quick and cost-free procedure, it appears that many women either perform it incorrectly or not at all.
Early diagnosis of breast cancer has been clearly shown to reduce mortality and improve survival8. Combined results from randomized screening trials suggest that mammography reduces the risk of dying from breast cancer by 15–20%, and studies of modern mammography screening programs in Europe found that the risk of death from breast cancer was reduced by more than one-third15. Thus, knowledge and practice of breast cancer preventive measures and screening is therefore critical in the reduction of breast cancer morbidity and mortality.
However, poor awareness and knowledge about breast cancer symptoms and screening methods have been previously reported by several different studies16. To plan critically needed breast cancer awareness and education programs that optimally address Nigerian women civil servants, healthcare professionals and planners must know the women’s current level of understanding. Therefore, this cross-sectional study in State Secretariat, Ibadan, was performed to explore public knowledge of breast self-examination (BSE) and mammogram amongst women workers in Oyo State.
Aims
The main aim of this study was to assess the level of knowledge and use of breast self-examination and mammogram among women of reproductive age in Oyo State Secretariat, Ibadan, Oyo State. Other objectives included: 1) Assess the level of knowledge of breast cancer, its risk factors and prevention measures; 2) Assess level of utilization of mammogram and breast self-examination; and 3) Identify the perceived barriers to the use of BSE and mammogram.
METHODS
Design
The study was a descriptive cross-sectional design that used a purposive sampling technique to select 204 consenting women from all specialities working in the State Secretariat, Agodi, Ibadan, to assess their views on breast cancer prevention actions (BSE and mammogram). Ethical approval was obtained from the Ethical Review Committee of the University of Ibadan, University College Hospital and from the Head of Service, Oyo State. With approval from the Head of Service, respondents’ consent was obtained, confidentiality of information was ensured and participants were not coerced to participate in the study and free to withdraw their participation at any stage of the study if they so desired without any negative consequences.
Sample
The subjects for the study were women workers of reproductive age (20–62 years) in Oyo State Secretariat, Agodi, Ibadan. The total number of female workers in Oyo State Secretariat were 340 and the sample size for this study was determined using the Yamane formula17. The calculated sample size was 184. Adjusting the sample size for 10% attrition, brought it to 204. Purposive sampling technique was used to select all participants who met the eligibility criteria.
Data collection
Data were collected using a structured validated close-ended questionnaire. The questionnaire consisted of five sections. Section A consisted of sociodemographic data. Section B asked questions on knowledge of breast cancer, its risk factors, signs and symptoms and preventive measures. Section C was on questions related to knowledge of BSE and mammogram. Section D was on level of utilization of mammogram and self-breast examination. Section E was concerned with barriers to the use of breast self-examination and mammogram.
The instrument was presented to research experts to ensure validity, while reliability was determined using a test-retest method among 10 female workers that were picked randomly from outside the study centre and yielded a coefficient of 0.75. The researchers administered the questionnaire to the respondents face-to-face and collected them after they were completed.
Data analysis
Data obtained were coded and entered into a spread-sheet. Analysis was performed using the Statistical Package for Social Science, version 20. Descriptive statistics such as frequency counts, percentages, mean and standard deviation were used to summarize and present the results. Student’s t-test was used to compare the categorical variables at p<0.05. Logistics regression was used to identify awareness and level of utilization of breast self-examination and mammogram among female workers in State Secretariat, Oyo State, at 0.05 level significance.
RESULTS
The 204 women who participated in the study had their questionnaires checked to ensure completion before retrieval. The return rate was 100%.
Of the respondents, 40.7% were in the age group 20–32 years (Table 1). Ethnic Yorubas represented the majority in the study consisting of 131 women (64.2%), while the least were 12 Hausas (5.9%). The majority (88.2%) had university education, while others (11.8%) were only diploma holders.
Table 1
Sociodemographic variables of the respondents
Knowledge on risk factors
Data on knowledge and risk of breast cancer revealed that 192 (94.1%) respondents heard about breast cancer, while 12 (5.9%), claimed they never heard of it. The sources of the 192 respondents’ information were: health workers (73, 38%), newspapers (71, 36.9%), parents (25, 13%), and social media (23, 12.1%). On the risk factors for breast cancer, 72 (37.5%) respondents reported genetics 23 (12.1%), diet 36 (18.6%), while others gave metaphysical reasons. On the symptoms, the majority 170 (88.6%) claimed a lump in the breast, change in breast shape 11 (5.7%) and shortness of breath. Genetic mutations were the most identified risk factor for breast cancer; 59 (30.7%) respondents claimed age, while 13 (6.8%) felt it resulted from post-menopausal hormone therapy.
The response of knowledge about the risk factors, causes, and symptoms of breast cancer showed that 17.2% (n=35) of the study population had poor knowledge of breast cancer and its risk factors. The cause, symptoms and risk factors of breast cancer were known by 82.8% (n=169) of the respondents. This means that the vast majority of women in the study had good knowledge of breast cancer. They were women who scored above the average of the total score, while those who scored below the average were women with poor knowledge (17.2%).
Table 2 gives the frequency and percentage distribution of respondents’ knowledge of BSE and mammogram and their significance in the prevention of breast cancer. The majority (66.2%) of the respondents agreed to go for breast cancer screening if they have a strong symptom, while the vast majority (94.1%) agreed to early screening being a good way of detecting breast cancer. Similarly, many (71.1%) knew that Magnetic Resonance Imaging is one method of screening for breast cancer. In the same way, many (77%) were aware of mammography and its usefulness in early detection of breast cancer.
Table 2
Frequency and percentage distribution of respondents’ knowledge of BSE and mammogram in the prevention of breast cancer (N=204)
Table 3 shows the level of utilization of the screening. More than half of the respondents (52.9%) did not practise breast self-examination at the age of 20 years, other (58.3%) respondents said they would never practise it. However, about half of the respondents were consistent with both the practice of BSE and mammogram, 47.1% and 58.8%, respectively.
Table 3
Frequency and percentage distributions of respondents’ level of utilization of mammogram and breast self-examination
Barriers and fears
On the barriers to using the mammogram and self-breast examination, 193 (94.6%) respondents maintained that breast cancer screening is time consuming. Fear of exposure to radiation discouraged 180 (88.2%) from doing mammography, while 122 (59.8%) claimed fear of the outcome of the mammogram and breast self-screening. Another 133 (65.2%) claimed they did not understand the process of breast self-examination and 168 (82.4%) suggested that they needed to know more about breast cancer screening.
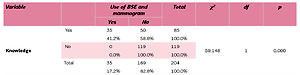
Table 4 shows that there is significant association between the knowledge of breast cancer and the use of BSE and mammogram (p<0.05). It also shows significant association between level of education and the use of BSE and mammogram (p<0.05). Hence, the null hypothesis was rejected.
Table 4
Cross-tabulation of respondents’ knowledge, level of education, and use of BSE and mammogram
DISCUSSION
The high level of knowledge demonstrated by the respondents is in agreement with studies in similar settings18,19, as well as in Turkey20. However, this level of knowledge is in contrast to other studies conducted in Turkey, where the majority of the women had little knowledge21, and among minorities in the United State22,23. Poor knowledge of the risk factors was also noted by studies in Nigeria24 and in the Middle East25-27.
Health workers and family members were the major sources of information on screening and knowledge of breast cancer according to researchers in similar settings28-30 while social media have also been identified as sources31. This view is also held by studies in developed countries32,33. However, information from family members and friends could be unreliable, thereby leading to fears and poor compliance. It is therefore important that oncology related health workers be trained in giving information to clients in various settings. This will be more correct, increase knowledge, improve use and reduce morbidity.
The fact that majority of the respondents were aware of the value of BSE in early detection of breast cancer and as a non-invasive procedure is in the right direction, in line with results from another study34, but in contrast with a study in a different setting33. Similarly, the participants’ knowledge of the value of mammography was supported by other studies. A Nigerian study noted that poor knowledge among their participants about mammography being an early detection measure24 was due to the fact that it was not readily available in a rural setting34. This could be attributed to the socioeconomic condition experienced in the countryside, especially among rural dwellers, where there is poor access, geographically and financially. Most of the rural dwellers are farmers with poor educational background that reduces their ability to access relevant information31. Also poor access roads prevent the sale of farm produce resulting in limited income, which further compounds the issue of knowledge about and travelling for a mammography. Improving accessibility to the rural areas could improve flow of information and increase knowledge of the value of a mammogram.
Findings from this study revealed low utilization of BSE and mammogram despite the high level of knowledge, in line with other studies23,30. However, an earlier study in the region found higher proportions of the practice of BSE but poor adherence to the process28,32. This could be attributed to increased awareness over the years, which led to more exposure but with no corresponding level of utilization. This suggests that the issue of wider utilization requires more than awareness and should be addressed by examining other sociocultural factors.
Among factors that constituted barriers were views of low risk and fear of having abnormal results; this has been corroborated by findings that views of not being at risk, fear, and anxiety of abnormal results are major barriers35. Also, the reported issue of not having enough time could be attributed to the long waiting experienced in most federal and state centers that offer screening services. The implication of this is that follow-up appointments should be streamlined in order to reduce waiting time and enhance compliance.
The issue of clinical and risk factors being significantly linked to respondents’ knowledge and educational level is in line with other studies36,37. A woman with a higher level of education is more likely to report promptly to the hospital for proper examination if any symptom suggestive of cancer is seen or felt; although earlier studies37,39 reported that educated women often forget to practise BSE.
Implication to nursing and midwifery practice
There is a need to educate women on BSE and mammography on the significance of the practice and use of these methods for the early detection of breast cancer. Nurses and midwives should organize training sessions, especially on BSE, so that women can practise it on their own.
CONCLUSIONS
Findings from this study demonstrate that although the majority of the respondents had adequate knowledge of BSE and mammogram, the level of utilization of these methods was still low. More so, a significant association was found between knowledge, level of education and use of BSE and mammogram. Identified barriers to wider utilization of the screening methods, were time, fears of the result of the screening, and other sociocultural factors, and these should be taken into account when designing interventions. This may reduce the barriers, facilitate wider utilization and ultimately lead to a decrease in the morbidity and mortality rate of breast cancer.
In as much as there are strategies in place for increasing awareness and sensitization about breast cancer screening, measures should also be in place to educate, motivate and encourage women to practise BSE and mammogram as preventive measures for the early detection of breast cancer.
Midwives should reinforce the need to practise these screening measures among women. Governments and other stake holders should provide support to facilitate the education of women and provide adequate information about preventive screening for breast cancer. Efforts should be directed to making mammogram more accessible, available and affordable for all, especially in rural areas.